Frequency
CLN3 disease is the most common type of NCL, but its exact prevalence is unknown; more than 400 cases have been described in the scientific literature. Collectively, all forms of NCL affect an estimated 1 in 100,000 individuals worldwide.
Causes
CLN3 disease is caused by mutations in the CLN3 gene, which provides instructions for making a protein that is found in tissues throughout the body. The CLN3 protein is part of many compartments within cells, including lysosomes, which are cellular compartments that digest and recycle different types of molecules. However, the exact function of the CLN3 protein is unclear. Research has shown that this protein is involved in many cellular processes, but it is uncertain which of them is the primary role of the protein, or if these processes instead represent downstream effects.
It is unclear how mutations in the CLN3 gene lead to the characteristic features of CLN3 disease. One CLN3 gene mutation, found in the vast majority of cases, leads to the production of an abnormally short protein. As a result, the abnormal CLN3 protein is broken down or may interfere with normal cellular processes. Other mutations reduce the amount of normal protein or impair its function. It is not known how loss of this protein causes the signs and symptoms of CLN3 disease.
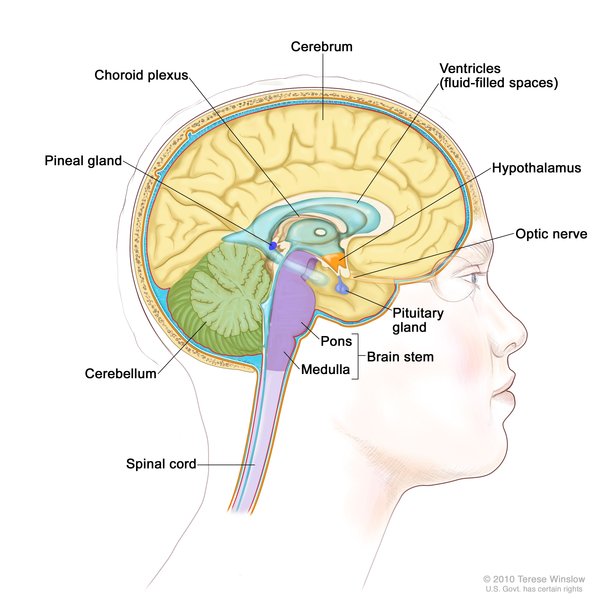
CLN3 disease, like other NCLs, is characterized by the accumulation of proteins and other substances in lysosomes. These accumulations occur in cells throughout the body; however, nerve cells seem to be particularly vulnerable to their effects. The accumulations can cause cell damage leading to cell death. The progressive death of nerve cells in the brain and other tissues leads to the neurological signs and symptoms of CLN3 disease. However, it is unclear how mutations in the CLN3 gene are involved in the buildup of substances in lysosomes.
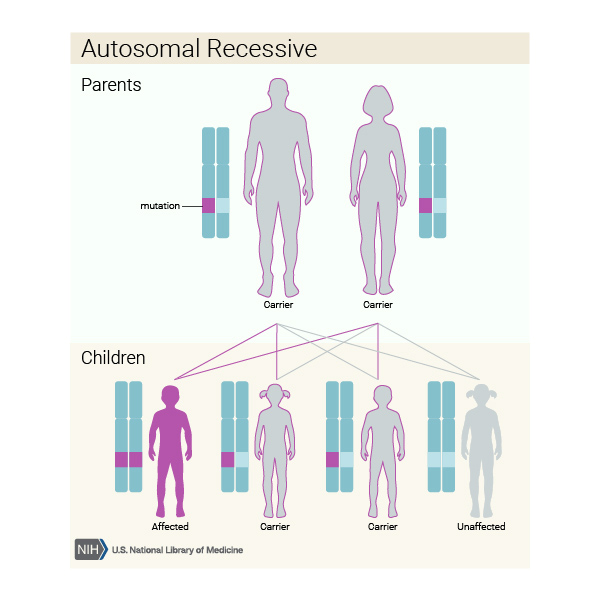
Inheritance
This condition is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
Other Names for This Condition
- Batten-Mayou disease
- Batten-Spielmeyer-Vogt disease
- CLN3-related neuronal ceroid-lipofuscinosis
- Juvenile Batten disease
- Juvenile cerebroretinal degeneration
- Juvenile neuronal ceroid lipofuscinosis
- Spielmeyer-Vogt disease
Additional Information & Resources
Genetic Testing Information
Genetic and Rare Diseases Information Center
Patient Support and Advocacy Resources
Clinical Trials
Catalog of Genes and Diseases from OMIM
Scientific Articles on PubMed
References
- Cotman SL, Staropoli JF. The juvenile Batten disease protein, CLN3, and its role in regulating anterograde and retrograde post-Golgi trafficking. Clin Lipidol. 2012 Feb;7(1):79-91. doi: 10.2217/clp.11.70. Citation on PubMed or Free article on PubMed Central
- Kollmann K, Uusi-Rauva K, Scifo E, Tyynela J, Jalanko A, Braulke T. Cell biology and function of neuronal ceroid lipofuscinosis-related proteins. Biochim Biophys Acta. 2013 Nov;1832(11):1866-81. doi: 10.1016/j.bbadis.2013.01.019. Epub 2013 Feb 9. Citation on PubMed
- Licchetta L, Bisulli F, Fietz M, Valentino ML, Morbin M, Mostacci B, Oliver KL, Berkovic SF, Tinuper P. A novel mutation af Cln3 associated with delayed-classic juvenile ceroid lipofuscinois and autophagic vacuolar myopathy. Eur J Med Genet. 2015 Oct;58(10):540-4. doi: 10.1016/j.ejmg.2015.09.002. Epub 2015 Sep 7. Citation on PubMed
- Mirza M, Vainshtein A, DiRonza A, Chandrachud U, Haslett LJ, Palmieri M, Storch S, Groh J, Dobzinski N, Napolitano G, Schmidtke C, Kerkovich DM. The CLN3 gene and protein: What we know. Mol Genet Genomic Med. 2019 Dec;7(12):e859. doi: 10.1002/mgg3.859. Epub 2019 Sep 30. Citation on PubMed or Free article on PubMed Central
- Oetjen S, Kuhl D, Hermey G. Revisiting the neuronal localization and trafficking of CLN3 in juvenile neuronal ceroid lipofuscinosis. J Neurochem. 2016 Nov;139(3):456-470. doi: 10.1111/jnc.13744. Epub 2016 Sep 9. Citation on PubMed
- Perez-Poyato MS, Mila Recansens M, Ferrer Abizanda I, Montero Sanchez R, Rodriguez-Revenga L, Cusi Sanchez V, Garcia Gonzalez MM, Domingo Jimenez R, Camino Leon R, Velazquez Fragua R, Martinez-Bermejo A, Pineda Marfa M. Juvenile neuronal ceroid lipofuscinosis: clinical course and genetic studies in Spanish patients. J Inherit Metab Dis. 2011 Oct;34(5):1083-93. doi: 10.1007/s10545-011-9323-7. Epub 2011 Apr 16. Citation on PubMed
- Rakheja D, Narayan SB, Bennett MJ. Juvenile neuronal ceroid-lipofuscinosis (Batten disease): a brief review and update. Curr Mol Med. 2007 Sep;7(6):603-8. doi: 10.2174/156652407781695729. Citation on PubMed
- Schulz A, Kohlschutter A, Mink J, Simonati A, Williams R. NCL diseases - clinical perspectives. Biochim Biophys Acta. 2013 Nov;1832(11):1801-6. doi: 10.1016/j.bbadis.2013.04.008. Epub 2013 Apr 17. Citation on PubMed or Free article on PubMed Central
- Williams RE, Mole SE. New nomenclature and classification scheme for the neuronal ceroid lipofuscinoses. Neurology. 2012 Jul 10;79(2):183-91. doi: 10.1212/WNL.0b013e31825f0547. Citation on PubMed
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.